Does Speech Motor Intervention Alter Brain Structure and Function?
As Speech-Language Pathologists, researchers and even caregivers of children with speech impairments, we have often wondered: “What does speech therapy actually do? Do we somehow change how the brain works?” Status appointed Adjunct Lecturer, Aravind Namasivayam, PhD from the Department of Speech-Language Pathology, University of Toronto and a co-author on two recent cortical plasticity papers on children with motor speech disorders proposes that “speech motor intervention does alter children’s brain structure, connectivity and function” (Chilosi et al., 2018; Fiori et al., 2018; Kadis et al., 2014; Yu et al., 2018).
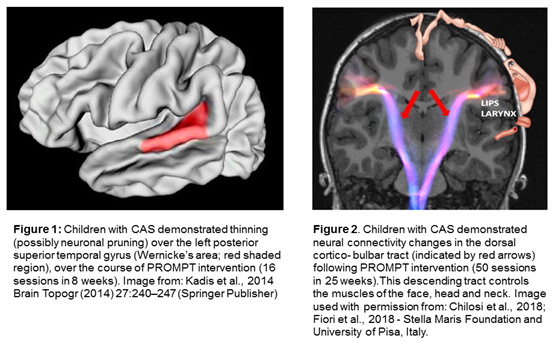 All children in the studies described below underwent a brief intensive motor speech intervention known as the Prompts for Restructuring Oral Muscular Phonetic Targets (PROMPT; Hayden et al., 2010). Kadis and colleagues (2014) at the Hospital for Sick Children and the University of Toronto used Magnetic Resonance Imaging (MRI) to demonstrate an intervention-induced thinning (or neural pruning) of the left posterior superior temporal gyrus (Wernicke’s area; Figure 1) in children with Childhood Apraxia of Speech (CAS; a form of speech sound disorder). Significant differences in magnetoencephalography (MEG) recordings of cortical neural activity (i.e., changes in neural firing patterns) was identified for children with speech sound disorders who received PROMPT, in regions related to motor speech control and speech production (Yu et al., 2014). In another study, Dr. Chilosi and colleagues (Chilosi et al., 2018; Fiori et al., 2018) from the Stella Maris Foundation and University of Pisa, Italy compared structural connectivity changes in white matter fiber tracts using Diffusion Tensor Imaging (DTI) in CAS participants receiving either PROMPT or Language and Non-Speech Oral Motor treatment. Interestingly, only in the PROMPT intervention group, changes in the behavioral measures were supported by increased neural plastic changes in the left dorsal corticobulbar tract that innervates the lip and facial muscles (Figure 2). In all studies, there was a significant improvement observed for behavioural measures of speech motor control and articulation in participants following treatment (Chilosi et al., 2018; Fiori et al., 2018; Kadis et al., 2014; Yu et al., 2018).
All children in the studies described below underwent a brief intensive motor speech intervention known as the Prompts for Restructuring Oral Muscular Phonetic Targets (PROMPT; Hayden et al., 2010). Kadis and colleagues (2014) at the Hospital for Sick Children and the University of Toronto used Magnetic Resonance Imaging (MRI) to demonstrate an intervention-induced thinning (or neural pruning) of the left posterior superior temporal gyrus (Wernicke’s area; Figure 1) in children with Childhood Apraxia of Speech (CAS; a form of speech sound disorder). Significant differences in magnetoencephalography (MEG) recordings of cortical neural activity (i.e., changes in neural firing patterns) was identified for children with speech sound disorders who received PROMPT, in regions related to motor speech control and speech production (Yu et al., 2014). In another study, Dr. Chilosi and colleagues (Chilosi et al., 2018; Fiori et al., 2018) from the Stella Maris Foundation and University of Pisa, Italy compared structural connectivity changes in white matter fiber tracts using Diffusion Tensor Imaging (DTI) in CAS participants receiving either PROMPT or Language and Non-Speech Oral Motor treatment. Interestingly, only in the PROMPT intervention group, changes in the behavioral measures were supported by increased neural plastic changes in the left dorsal corticobulbar tract that innervates the lip and facial muscles (Figure 2). In all studies, there was a significant improvement observed for behavioural measures of speech motor control and articulation in participants following treatment (Chilosi et al., 2018; Fiori et al., 2018; Kadis et al., 2014; Yu et al., 2018).
Dr. Namasivayam is thrilled about these findings, as it is the first to explain how and why a speech motor intervention produces its effects, referred to as a Mode of Action (MoA). Demonstration of MoA is key component of discovery and development of therapeutic intervention with federal agencies like the U.S. Food and Drug Administration (www.fda.gov). He suggests that the discovery of MoA for motor speech intervention (specifically PROMPT) in children will (with further research) allow us to (1) identify populations with speech disorders that are most likely to respond to intervention, (2) modify intervention procedures (such as dosage) to replicate the neural effects, and (3) monitor and avoid adverse neural and behavioural outcomes.
References
Chilosi, A., Podda, I., Fiori, S., Pannek, K., Franchi, B., & Cipriani, P. (2018). Whole brain connectivity in childhood apraxia of speech and the effects of intervention. Presented at the 19th Biennial Conference on Motor Speech, Savannah, GA, February 22-25, 2018. Savannah, GA.
Fiori, S., Pannek, K., Podda, I., Cipriani, P., Franchi, B., Pasquariello, R., … Chilosi, A. (2018). Neural plasticity induced by a speech motor treatment in CAS: Preliminary results. Manuscript submitted for publication.
Hayden, D., Eigen, J., Walker, A., & Olsen, L. (2010). PROMPT: A tactually grounded model for the treatment of childhood speech production disorders. In Williams, L.; McLeod, S.; McCauley, R., (Eds.). Treatment for speech sound disorders in children (pp. 453-474). Baltimore, MD: Brookes Publishing.
Kadis D. S., Goshulak D., Namasivayam A., Pukonen M., Kroll R., De Nil L. F., … Lerch, J. P. (2014). Cortical thickness in children receiving intensive therapy for idiopathic apraxia of speech. Brain Topography, 27(2), 240-247.
Yu, V. Y., Kadis, D. S., Goshulak, D., Namasivayam, A., Pukonen, M., Kroll, R., …Pang, E.W. (2018). Impact of motor speech intervention on neural activity in children with speech sound disorders: Use of magnetoencephalography. Journal of Behavioral and Brain Science, 8, 415-429.